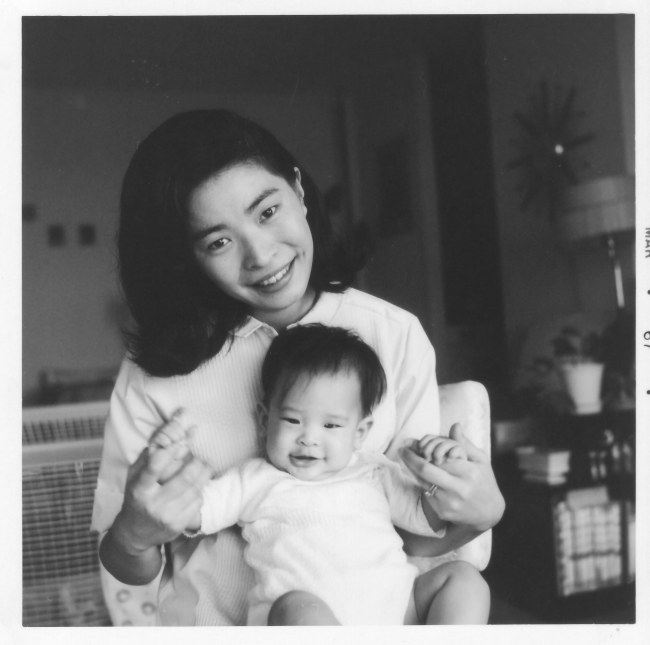
This is my mom. Please spend a moment and look upon her beautiful face. Perhaps you may see some of the same qualities that I do: the hopeful happiness in her smile, the joyful but fiery intensity in her eyes, the serene youthfulness in her gaze. She looks so young and new here, new at adulthood, parenthood, American life. But for me, her son, I also see wisdom, awareness, a vague sense of knowing, some ill-defined proficiency in everything she does, though she was much newer at this parenting thing when the photo was taken than I am now. A lifetime of observing my mom’s way of being and burning love for her family gives me well-informed license to perceive these special qualities: this unique perspective creates a sensation, and feeling you cannot know unless it’s your own mother you see looking back at you from that old, black-and-white photograph.
Mom had gone through a lot to get to where she was when my dad snapped this photo. She had left her native country and a life of comfort and stability–a true rarity in Korea at the time–for a modest life with a young Japanese-born, American-trained professor of Korean descent, now living and teaching in Michigan. An accomplished pianist and young scholar in her own right, she threw herself eagerly into the responsibilities of being a wife and parent, managing to earn a master’s degree in mathematics along the way. Looking at her young, smiling face, one wonders if she had some inkling of the adventures to come: all the soccer and baseball games, the world travel, the many times playing hostess to friends and her husband’s many colleagues and students, the maturation and graduation of her sons, the germination and success of her businesses.
She could not have known, however, about all the challenges that lay ahead. Apart from the passing of my father–the most devastating event in the lives of everybody in my immediate family–the biggest challenge of them all was her diagnosis with Parkinson disease, which has over the past several years gradually robbed her of her agility, coordination, and ability to walk.
A neurologist by training, I have counseled many patients and families regarding the management of Parkinson disease over the years. No clinical experience or medical training could compare, however, to the education I have received from helping a parent cope with this cruel disorder every day. It has been a truly humbling experience, realizing the true personal effects of Parkinson’s as I have through my mother. This knowledge now in hand and without dwelling on details, I am qualified to offer this one, non-doctorly piece of simple, universal advice: never get Parkinson’s. It blows.
Today’s entry pertains to sleep because Mom started having substantial insomnia–without a clear trigger–years prior to her diagnosis with Parkinson’s. Parkinson disease is commonly associated with sleep disruption and it is not uncommon for the first symptoms of Parkinson’s to be very nonspecific, starting well prior to the onset of more specific symptoms (tremor, slowness of movements, and the like), so I wonder in retrospect if her difficulties sleeping represented the heralding problem of her particular disorder. Her neurologist, a movement disorder specialist, is doing what she can to manage the insomnia, but Mom still struggles with her sleep from time to time.
Last year I had the pleasure of introducing my mother to Michael J. Fox, whose public battle with early-onset Parkinson disease has been the inspiration for many public speaking events and several excellent, highly recommended books (which Mom and I have both read), including Lucky Man: A Memoir and Always Looking Up: The Adventures of an Incurable Optimist. Mr. Fox told Mom, “You look great!” It was wonderful for her to meet someone who has lived what she is living, someone who understands. She smiled quietly in response, and in her expression I saw that same hope and determination she’s always had, qualities so relentlessly challenged in recent years by this crippling disorder. I believe that that fight will always be there, despite the fatigue, because that’s who she is and who she will always be. And my family and I will continue to be there for her, helping her fight. When it comes to my mom, I took off my doctor’s hat long ago. I’m just a son, a boy loving and trying to help his parent. That’s all I can be now, and I think that’s what she needs most.
Today’s Mother’s Day. Dang it, man. Love your mom. Remember her if she’s gone. Squeeze her tight if she’s not. Call her if she’s away. Just don’t waste a second of her presence. Moms are incredibly precious. I know mine is.